Everyday heart health tips | Health | iDiva.com
With sedentary jobs and increasing deadlines, we don't end up paying enough attention to our hearts. Cardiovascular disease in India has quadrupled in the last 40 years and WHO estimates that by 2020 close to 60 percent of cardiac patients worldwide will be Indian [source: expresspharmaonline.com].
Don't lose hope yet! Dr Ramakant Panda, who was awarded the Padma Bhushan this year and has had the oppurtunity to operate on Prime Minister Manmohan Singh gives you tips to follow everyday to make your heart healthier.
1. 5-a-day: Eat at least 5 servings of fresh fruits and vegetables for a healthier heart.
2. Banish that salt shaker from the dinner table. Never add extra salt on top of your food. Excess sodium intake causes hypertension.
3. If you must drink, ensure that it's no more than 2 drinks a day for men and a drink a day for women.
4. Walk for your heart. It's the best heart healthy exercise and will not cost you a rupee. Every step you take during the day builds up your heart balance & helps prevent disease.
5. Take the stairs for a healthier heart. When you go up, your blood pressure goes down.
6. Quit today. Thousands of Indians quit smoking everyday - by dying. Save your heart and lungs. Smoking also speeds up the development of plaque in the arteries.
7. Start slowly. Build up to at least 30 minutes of activity, five times per week. Try two 15-minute sessions or three 10-minute sessions to meet your goal. However, don't exercise right after meals, or when it's very hot and humid. Always warm-up before exercise and cool down after you are done.
8. Substitute lower-fat foods for higher-fat ones. Some examples include skim or 1% milk for whole milk. Saturated fats are typically solid at room temperature. Try the squeeze test: the firmer the fat, the more it's saturated. AVOID AT ALL COSTS!
9. Reduce your sodium intake to no more than 2400 mg of sodium or 1 1/4 teaspoons of salt per day.
10. Know your numbers - The first step towards better heart health is to know where you stand currently. For that it is very important for you to know your health numbers. Get your lipid profile, blood sugar levels and BP regularly checked. Have regular physical exams that include tests to see if, your are at risk for cardiovascular disease
11. Don't let the weighing scale rule you- It is important to maintain a healthy weight, according to your height, but it is more important to eat a healthful diet & exercise regularly.
12. Follow your grandparents- Every day fad diets spring up, and foods tend to go in and out of fashion, as fast as clothes. The 'sensible diet' preached and followed by our forefathers is the best for health. Eat healthy & don't crash diet
13. Get yourself checked- Keep a tab on your last visit to your Doctor. Don't miss your follow-ups. It is always advisable to go in for a complete health checkup at least once a year.
14. Sugar is not so sweet- If you have diabetes, keep the blood sugars under 'tight control'. Remember, physical activity is the best way to burn off excess sugar in the blood. Those with diabetes are more prone to heart disease, especially women.
Saturday, April 10, 2010
Sunday, April 4, 2010
Physical health
Get the facts on sexual health screening, contraception and sexually transmitted infections.
Sexually transmitted infections
Chlamydia
Gonorrhoea
Genital herpes
Pubic lice
Scabies
NSU
HIV
Syphilis
Trichomonas vaginalis
Thrush
Genital warts
To prevent sexually transmitted infections as well as pregnancy you must use a barrier method of contraception. This fpa factsheet describes one of the most popular - condoms.
What are they?
Condoms are barrier methods that prevent sperm meeting an egg. There are male and female condoms. Condoms are made of latex (rubber) or polyurethane (plastic).
Advantages:
Very effective
Easily available (male condoms)
Only need to use them when you have sex
Help to protect against some sexually transmitted infections (STIs), including HIV
Male condoms come in many different varieties, shapes and sizes
Female condoms can be put in at any time before sex
Disadvantages:
Can interrupt sex
Male condoms can slip off or split if used incorrectly
When using the female condom care is needed to ensure the penis goes inside the condom and not down the side of the condom and the vagina
Some people are sensitive to the chemicals in latex condoms, although this is not common
Oil-based lubricants, such as body oils or lotions, should not be used with latex condoms
Sexually transmitted infections
Chlamydia
Gonorrhoea
Genital herpes
Pubic lice
Scabies
NSU
HIV
Syphilis
Trichomonas vaginalis
Thrush
Genital warts
To prevent sexually transmitted infections as well as pregnancy you must use a barrier method of contraception. This fpa factsheet describes one of the most popular - condoms.
What are they?
Condoms are barrier methods that prevent sperm meeting an egg. There are male and female condoms. Condoms are made of latex (rubber) or polyurethane (plastic).
Advantages:
Very effective
Easily available (male condoms)
Only need to use them when you have sex
Help to protect against some sexually transmitted infections (STIs), including HIV
Male condoms come in many different varieties, shapes and sizes
Female condoms can be put in at any time before sex
Disadvantages:
Can interrupt sex
Male condoms can slip off or split if used incorrectly
When using the female condom care is needed to ensure the penis goes inside the condom and not down the side of the condom and the vagina
Some people are sensitive to the chemicals in latex condoms, although this is not common
Oil-based lubricants, such as body oils or lotions, should not be used with latex condoms
No Diet diet PLAN
Here are the DOs
Do eat 3 moderate-sized meals a day, breakfast, lunch and dinner.
Watch the amount of you drink
Do limit your alcohol consumption to 3 units of alcohol per day.
Do look at the nutritional labels on food. Only buy products that contain 4 grams or less of fat per 100 grams (4% fat).
Do increase your activity levels. Use the stairs more, walk further and more often. Try the walking programme and the fat burner workout.
Do cut out all visible fat from your diet. That includes butter, margarine, oils and mayonnaise.
Do eat a desert if you want to. Just select a low-fat (max. 4% fat) pudding.
Vegetables help to bulk up your main meal
Do eat enough at mealtimes to fill you up. Vegetables are great fillers with your main meal.
Do eat 3 pieces of fruit per day.
Do drink 300ml (1/2 pint) of semi- skimmed milk each day, this can be in your hot drinks and on your cereal.
Do drink as much water as possible. Diet drinks are also unrestricted.
Do continue to dine out, but avoid anything fried, coated in breadcrumbs or batter or cooked in pastry.
Eating out at a restaurant - beware of the pitfalls! Choose a jacket potato or boiled potato in preference to chips. Ask for your food to be cooked without fat and have fat-free dressings.
Do choose soup as a starter as it is a good filler. Avoid creamy soups and forget the bread roll.
Do weigh yourself and measure your waist every week at the same time of day, under the same conditions. Wear the same and use the same scales. Keep a record of your progress.
Do balance the effects of a sumptuous meal out by taking extra exercise the next day.
Do cook and serve all food without adding fat.
And the DON'Ts
Don't nibble between meals.
Avoid the sweet counter to keep your waistline trim
Don't buy any chocolate or sweets.
Don't save up your daily alcohol allowance and drink it in one go.
Don't skip meals.
Don't eat just one massive meal a day.
Don't eat biscuits, cakes, pastries - in fact anything with more than 4% fat content, except oily fish.
The weight loss will not be as fast as following a set diet.
Do eat 3 moderate-sized meals a day, breakfast, lunch and dinner.
Watch the amount of you drink
Do limit your alcohol consumption to 3 units of alcohol per day.
Do look at the nutritional labels on food. Only buy products that contain 4 grams or less of fat per 100 grams (4% fat).
Do increase your activity levels. Use the stairs more, walk further and more often. Try the walking programme and the fat burner workout.
Do cut out all visible fat from your diet. That includes butter, margarine, oils and mayonnaise.
Do eat a desert if you want to. Just select a low-fat (max. 4% fat) pudding.
Vegetables help to bulk up your main meal
Do eat enough at mealtimes to fill you up. Vegetables are great fillers with your main meal.
Do eat 3 pieces of fruit per day.
Do drink 300ml (1/2 pint) of semi- skimmed milk each day, this can be in your hot drinks and on your cereal.
Do drink as much water as possible. Diet drinks are also unrestricted.
Do continue to dine out, but avoid anything fried, coated in breadcrumbs or batter or cooked in pastry.
Eating out at a restaurant - beware of the pitfalls! Choose a jacket potato or boiled potato in preference to chips. Ask for your food to be cooked without fat and have fat-free dressings.
Do choose soup as a starter as it is a good filler. Avoid creamy soups and forget the bread roll.
Do weigh yourself and measure your waist every week at the same time of day, under the same conditions. Wear the same and use the same scales. Keep a record of your progress.
Do balance the effects of a sumptuous meal out by taking extra exercise the next day.
Do cook and serve all food without adding fat.
And the DON'Ts
Don't nibble between meals.
Avoid the sweet counter to keep your waistline trim
Don't buy any chocolate or sweets.
Don't save up your daily alcohol allowance and drink it in one go.
Don't skip meals.
Don't eat just one massive meal a day.
Don't eat biscuits, cakes, pastries - in fact anything with more than 4% fat content, except oily fish.
The weight loss will not be as fast as following a set diet.
Saturday, October 24, 2009
VIRUS
Swine influenza (also called swine flu, hog flu, pig flu and sometimes, the swine) is an infection by any one of several types of swine influenza virus. Swine influenza virus (SIV) is any strain of the influenza family of viruses that is endemic in pigs. As of 2009, the known SIV strains include influenza C and the subtypes of influenza A known as H1N1, H1N2, H3N1, H3N2, and H2N3.
Swine influenza virus is common throughout pig populations worldwide. Transmission of the virus from pigs to humans is not common and does not always lead to human influenza, often resulting only in the production of antibodies in the blood. If transmission does cause human influenza, it is called zoonotic swine flu. People with regular exposure to pigs are at increased risk of swine flu infection. The meat of an infected animal poses no risk of infection when properly cooked.
During the mid-20th century, identification of influenza subtypes became possible, allowing accurate diagnosis of transmission to humans. Since then, only 50 such transmissions have been confirmed. These strains of swine flu rarely pass from human to human. Symptoms of zoonotic swine flu in humans are similar to those of influenza and of influenza-like illness in general, namely chills, fever, sore throat, muscle pains, severe headache, coughing, weakness and general discomfort.
Pandemic H1N1/09 virus.
The Pandemic H1N1/09 virus is a swine origin Influenza A virus subtype H1N1 virus strain responsible for the 2009 flu pandemic.
Electron microscope image of the reassorted H1N1 influenza virus photographed at the CDC Influenza Laboratory. The viruses are 80–120 nanometres in diameter

Contagiousness
The virus is contagious and is believed to spread from human to human in much the same way as seasonal flu. The most common mechanisms by which it spreads are by droplets from coughs and sneezes of infected people, and touching a surface or the hand of a person contaminated with virus, and then touching one's mouth or nose.H1N1/09 is more contagious than seasonal flu[11], and infected people are contagious for longer than had been thought. The US CDC had recommended that people should wait at least a day after their fever subsides (usually 3–4 days after the onset of symptoms) before resuming normal activities, but it has been found that they can continue to shed virus for several days after that.[12]
The contagiousness of the virus may change as it mutates.
Vaccine
Main article: 2009 flu pandemic vaccine
Existing vaccines against seasonal flu provide no protection, but as of September 2009 a vaccine for H1N1/09 is in an advanced stage of development, with delivery expected to start in November 2009, although production may be 3 billion doses per year rather than the earlier estimate of 5 billion.
Initial Phase I human testing began with Novartis' MF59 candidate in July 2009, at which time phase II trials of CSL's candidate CSL425 vaccine were planned to start in August 2009, but had not begun recruiting. Sanofi Pasteur's candidate inactivated H1N1 had several phase II trials planned as of 21 July 2009, but had not begun recruiting. News coverage conflicted with this information, as Australian trials of the CSL candidate were announced as having started on 21 July and the Chinese government announce the start of trials of the Hualan Biological Engineering candidate.
Pandemrix, made by GlaxoSmithKline (GSK), was approved by the European Medicines Agency on 25 September 2009, and Baxter's vaccine has been reported as likely to get approved the following week. The first comparative clinical study of both vaccines started on children in the UK on 25 September.
Arepanrix, an adjuvanted vaccine made by GSK, was authorized by Canada's Minister of Health on 21 October 2009.
Swine influenza virus is common throughout pig populations worldwide. Transmission of the virus from pigs to humans is not common and does not always lead to human influenza, often resulting only in the production of antibodies in the blood. If transmission does cause human influenza, it is called zoonotic swine flu. People with regular exposure to pigs are at increased risk of swine flu infection. The meat of an infected animal poses no risk of infection when properly cooked.
During the mid-20th century, identification of influenza subtypes became possible, allowing accurate diagnosis of transmission to humans. Since then, only 50 such transmissions have been confirmed. These strains of swine flu rarely pass from human to human. Symptoms of zoonotic swine flu in humans are similar to those of influenza and of influenza-like illness in general, namely chills, fever, sore throat, muscle pains, severe headache, coughing, weakness and general discomfort.
Pandemic H1N1/09 virus.
The Pandemic H1N1/09 virus is a swine origin Influenza A virus subtype H1N1 virus strain responsible for the 2009 flu pandemic.
Electron microscope image of the reassorted H1N1 influenza virus photographed at the CDC Influenza Laboratory. The viruses are 80–120 nanometres in diameter

Contagiousness
The virus is contagious and is believed to spread from human to human in much the same way as seasonal flu. The most common mechanisms by which it spreads are by droplets from coughs and sneezes of infected people, and touching a surface or the hand of a person contaminated with virus, and then touching one's mouth or nose.H1N1/09 is more contagious than seasonal flu[11], and infected people are contagious for longer than had been thought. The US CDC had recommended that people should wait at least a day after their fever subsides (usually 3–4 days after the onset of symptoms) before resuming normal activities, but it has been found that they can continue to shed virus for several days after that.[12]
The contagiousness of the virus may change as it mutates.
Vaccine
Main article: 2009 flu pandemic vaccine
Existing vaccines against seasonal flu provide no protection, but as of September 2009 a vaccine for H1N1/09 is in an advanced stage of development, with delivery expected to start in November 2009, although production may be 3 billion doses per year rather than the earlier estimate of 5 billion.
Initial Phase I human testing began with Novartis' MF59 candidate in July 2009, at which time phase II trials of CSL's candidate CSL425 vaccine were planned to start in August 2009, but had not begun recruiting. Sanofi Pasteur's candidate inactivated H1N1 had several phase II trials planned as of 21 July 2009, but had not begun recruiting. News coverage conflicted with this information, as Australian trials of the CSL candidate were announced as having started on 21 July and the Chinese government announce the start of trials of the Hualan Biological Engineering candidate.
Pandemrix, made by GlaxoSmithKline (GSK), was approved by the European Medicines Agency on 25 September 2009, and Baxter's vaccine has been reported as likely to get approved the following week. The first comparative clinical study of both vaccines started on children in the UK on 25 September.
Arepanrix, an adjuvanted vaccine made by GSK, was authorized by Canada's Minister of Health on 21 October 2009.
Saturday, October 17, 2009
LIVER DISORDER
Jaundice, also known as icterus (attributive adjective: icteric), is a yellowish discoloration of the skin, the conjunctival membranes over the sclerae (whites of the eyes), and other mucous membranes
Monday, August 31, 2009
DENTAL SURGEON
Dentistry is the known evaluation, diagnosis, prevention, and treatment of diseases, disorders and conditions of the soft and hard tissues of the jaw (mandible), the oral cavity, maxillofacial area and the adjacent and associated structures and their impact on the human body. Dentistry is widely considered necessary for complete overall health. Those in the practice of dentistry are known as dentists. Other people aiding in oral health service include dental assistants, dental hygienists, dental technicians, and dental therapists.
Dentistry is that branch of medicine which deals with the study and practice of diagnosis, prevention, and treatment of diseases of the mouth, the maxilla, and the face.
The first dental school, Baltimore College of Dental Surgery opened in Baltimore, Maryland, USA in 1840, and in 1867, Harvard Dental School became the second dental school affiliated with a university.
Official specialties
Dental public health (study of dental epidemiology and social health policies),
Endodontics (root canal therapy and study of diseases of the dental pulp),
Oral and Maxillofacial Pathology (study, diagnosis, and sometimes the treatment of oral and maxillofacial related diseases),
Oral and Maxillofacial Radiology (study and radiologic interpretation of oral and maxillofacial diseases),
Oral and Maxillofacial Surgery (extractions, implants, and facial surgery),
Orthodontics and Dentofacial Orthopaedics (straightening of teeth and modification of midface and mandibular growth),
Periodontics (study and treatment of diseases of the periodontium (non-surgical and surgical), and placement and maintenance of dental implants),
Pediatric dentistry (i.e. dentistry for children, formerly known as "pedodontics"),
Prosthodontics (dentures, bridges and the restoration of implants. Some prosthodontists further their training in "oral and maxillofacial prosthodontics"--a discipline concerned with the replacement of missing facial structures—such as ears, eyes, nose, etc.)
History
The Indus Valley Civilization in Pakistan has yielded evidence of dentistry being practiced as far back as 7000 BCE. This earliest form of dentistry involved curing tooth related disorders with bow drills operated, perhaps, by skilled bead craftsmen.[18] The reconstruction of this ancient form of dentistry showed that the methods used were reliable and effective.
A Sumerian text from 5000 BC describes a "tooth worm" as the cause of dental caries.[20] Evidence of this belief has also been found in ancient India, Egypt, Japan, and China. The legend of the worm is also found in the writings of Homer, and as late as the 1300s AD the surgeon Guy de Chauliac still promoted the belief that worms cause tooth decay.
The Edwin Smith Papyrus, written in the 17th century BC but which may reflect previous manuscripts from as early as 3000 BC, includes the treatment of several dental ailments. In the 18th century BC, the Code of Hammurabi referenced dental extraction twice as it related to punishment. Examination of the remains of some ancient Egyptians and Greco-Romans reveals early attempts at dental prosthetics and surgery.
Ancient Greek scholars Hippocrates and Aristotle wrote about dentistry, including the eruption pattern of teeth, treating decayed teeth and gum disease, extracting teeth with forceps, and using wires to stabilize loose teeth and fractured jaws The first use of dental appliances or bridges comes from the Etruscans from as early as 700BC. Roman medical writer Cornelius Celsus wrote extensively of oral diseases as well as dental treatments such as narcotic-containing emollients and astringents.
Historically, dental extractions have been used to treat a variety of illnesses. During the Middle Ages and throughout the 19th century, dentistry was not a profession in itself, and often dental procedures were performed by barbers or general physicians. Barbers usually limited their practice to extracting teeth which alleviated pain and associated chronic tooth infection. Instruments used for dental extractions date back several centuries. In the 14th century, Guy de Chauliac invented the dental pelican(resembling a pelican's beak) which was used up until the late 18th century. The pelican was replaced by the dental key which, in turn, was replaced by modern forceps in the 20th century.[citation needed]
The first book focused solely on dentistry was the "Artzney Buchlein" in 1530, and the first dental textbook written in English was called "Operator for the Teeth" by Charles Allen in 1685. It was between 1650 and 1800 that the science of modern dentistry developed. It is said that the 17th century French physician Pierre Fauchard started dentistry science as we know it today, and he has been named "the father of modern dentistry". Among many of his developments were the extensive use of dental prosthesis, the introduction of dental fillings as a treatment for dental caries and the statement that sugar derivate acids such as tartaric acid are responsible for dental decay.
Dentistry is that branch of medicine which deals with the study and practice of diagnosis, prevention, and treatment of diseases of the mouth, the maxilla, and the face.
The first dental school, Baltimore College of Dental Surgery opened in Baltimore, Maryland, USA in 1840, and in 1867, Harvard Dental School became the second dental school affiliated with a university.
Official specialties
Dental public health (study of dental epidemiology and social health policies),
Endodontics (root canal therapy and study of diseases of the dental pulp),
Oral and Maxillofacial Pathology (study, diagnosis, and sometimes the treatment of oral and maxillofacial related diseases),
Oral and Maxillofacial Radiology (study and radiologic interpretation of oral and maxillofacial diseases),
Oral and Maxillofacial Surgery (extractions, implants, and facial surgery),
Orthodontics and Dentofacial Orthopaedics (straightening of teeth and modification of midface and mandibular growth),
Periodontics (study and treatment of diseases of the periodontium (non-surgical and surgical), and placement and maintenance of dental implants),
Pediatric dentistry (i.e. dentistry for children, formerly known as "pedodontics"),
Prosthodontics (dentures, bridges and the restoration of implants. Some prosthodontists further their training in "oral and maxillofacial prosthodontics"--a discipline concerned with the replacement of missing facial structures—such as ears, eyes, nose, etc.)
History
The Indus Valley Civilization in Pakistan has yielded evidence of dentistry being practiced as far back as 7000 BCE. This earliest form of dentistry involved curing tooth related disorders with bow drills operated, perhaps, by skilled bead craftsmen.[18] The reconstruction of this ancient form of dentistry showed that the methods used were reliable and effective.
A Sumerian text from 5000 BC describes a "tooth worm" as the cause of dental caries.[20] Evidence of this belief has also been found in ancient India, Egypt, Japan, and China. The legend of the worm is also found in the writings of Homer, and as late as the 1300s AD the surgeon Guy de Chauliac still promoted the belief that worms cause tooth decay.
The Edwin Smith Papyrus, written in the 17th century BC but which may reflect previous manuscripts from as early as 3000 BC, includes the treatment of several dental ailments. In the 18th century BC, the Code of Hammurabi referenced dental extraction twice as it related to punishment. Examination of the remains of some ancient Egyptians and Greco-Romans reveals early attempts at dental prosthetics and surgery.
Ancient Greek scholars Hippocrates and Aristotle wrote about dentistry, including the eruption pattern of teeth, treating decayed teeth and gum disease, extracting teeth with forceps, and using wires to stabilize loose teeth and fractured jaws The first use of dental appliances or bridges comes from the Etruscans from as early as 700BC. Roman medical writer Cornelius Celsus wrote extensively of oral diseases as well as dental treatments such as narcotic-containing emollients and astringents.
Historically, dental extractions have been used to treat a variety of illnesses. During the Middle Ages and throughout the 19th century, dentistry was not a profession in itself, and often dental procedures were performed by barbers or general physicians. Barbers usually limited their practice to extracting teeth which alleviated pain and associated chronic tooth infection. Instruments used for dental extractions date back several centuries. In the 14th century, Guy de Chauliac invented the dental pelican(resembling a pelican's beak) which was used up until the late 18th century. The pelican was replaced by the dental key which, in turn, was replaced by modern forceps in the 20th century.[citation needed]
The first book focused solely on dentistry was the "Artzney Buchlein" in 1530, and the first dental textbook written in English was called "Operator for the Teeth" by Charles Allen in 1685. It was between 1650 and 1800 that the science of modern dentistry developed. It is said that the 17th century French physician Pierre Fauchard started dentistry science as we know it today, and he has been named "the father of modern dentistry". Among many of his developments were the extensive use of dental prosthesis, the introduction of dental fillings as a treatment for dental caries and the statement that sugar derivate acids such as tartaric acid are responsible for dental decay.
BONE DISORDER
Osteomyelitis , is an infection of bone or bone marrow with a propensity for progression, usually caused by pyogenic bacteria or mycobacteria .

Osteomyelitis of the tibia of a young child. Numerous abscesses in the bone show as radiolucency
Osteomyelitis is an infective process which encompasses all of the bone (osseous) components, including the bone marrow. When it is chronic it can lead to bone sclerosis and deformity.
Age group Most common organisms
Newborns (younger than 4 mo) S. aureus, Enterobacter species, and group A and B Streptococcus species
Children (aged 4 mo to 4 y) S. aureus, group A Streptococcus species, Haemophilus influenzae, and Enterobacter species
Children, adolescents (aged 4 y to adult) S. aureus (80%), group A Streptococcus species, H. influenzae, and Enterobacter species
Adult S. aureus and occasionally Enterobacter or Streptococcus species

Osteomyelitis of the tibia of a young child. Numerous abscesses in the bone show as radiolucency
Osteomyelitis is an infective process which encompasses all of the bone (osseous) components, including the bone marrow. When it is chronic it can lead to bone sclerosis and deformity.
Age group Most common organisms
Newborns (younger than 4 mo) S. aureus, Enterobacter species, and group A and B Streptococcus species
Children (aged 4 mo to 4 y) S. aureus, group A Streptococcus species, Haemophilus influenzae, and Enterobacter species
Children, adolescents (aged 4 y to adult) S. aureus (80%), group A Streptococcus species, H. influenzae, and Enterobacter species
Adult S. aureus and occasionally Enterobacter or Streptococcus species
Tuesday, October 7, 2008
TOOTH PAIN
When do you need a root canal treatment'
If there is inflammation and swelling, the DENTAL SURGEON/ ENDODONTIST may prescribe an antibiotic or/and anti-inflammatory medicine for some days before starting the root canal procedure. The purpose is to control the infection and to ease the swelling which can make the anesthetic less effective.
If the condition is painful, the patient will have to take an over the counter or prescription analgesic to relieve the tooth pain until the procedure. The next step in the procedure is to take an X-ray to check the shape of the root canals and determine if there are any signs of infection in the surrounding bone
At the center of a tooth is a hollow area that houses soft tissue, known as pulp. This hollow area contains a relatively wide space towards the chewing surface of the tooth called the pulp chamber. This chamber is connected to the tip of the root of the tooth via thin hollow pipe-like canals—hence, the term "root canal". Human teeth normally have one to four canals, with teeth toward the back of the mouth having the most. These canals run through the center of the roots like pencil lead runs through the length of a pencil. The tooth receives nutrition through the blood vessels and nerves traversing these canals.
For patients, root canal therapy is one of the most feared procedures in all of dentistry; however, dental professionals assert that modern root canal treatment is relatively painless because the pain can be controlled. Lidocaine is a commonly used local anaesthetic. Pain control medication may be used either before or after treatment. However, in some cases it may be very difficult to achieve pain control before performing a root canal. For example, if a patient has an abscessed tooth, with a swollen area or "fluid-filled gum blister" next to the tooth, the pus in the abscess may contain acids that inactivate any anaesthetic injected around the tooth. In this case, it is best for the DOCTOR to drain the abscess by cutting it to let the pus drain out. Releasing the pus releases pressure built up around the tooth; this pressure causes much pain. The DENTAL SURGEON then prescribes a week of antibiotics such as penicillin, which will reduce the infection and pus, making it easier to anaesthetise the tooth when the patient returns one week later. The DENTAL SURGEON could also open up the tooth and let the pus drain through the tooth, and could leave the tooth open for a few days to help relieve pressure.
Steps of the Root Canal Procedure
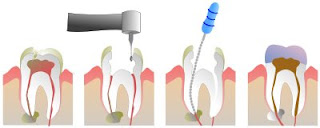
Root canal procedure'
1. Preparation for a root canal treatment
2. Anesthesia
3. Isolating the tooth
4. Gaining access to the dental pulp
5. Removal of PULP TISSUE
6. Measuring
7. Cleaning the root canals
8. Filling the root canals

Lower right first molar (center) after root canal therapy; the pulp chamber and root canals have been cleaned of debris, decontaminated and filled with gutta percha.
9.Restoring the Tooth After Root Canal
PULPECTOMY "pulpectomy" Sometimes the DENTAL SURGEON performs preliminary treatment of the tooth by removing all of the infected pulp of the tooth and applying a dressing and temporary filling to the tooth.
PULPOTOMY "pulpotomy" The DENTAL SURGEON may also remove just the coronal portion of the dental pulp, which contains 90% of the nerve tissue, and leave intact the pulp in the canals. This procedure, called a "pulpotomy", tends to essentially eliminate all the pain .
The pulpectomy and pulpotomy procedures eliminate almost all pain until the follow-up visit for finishing the root canal. But if the pain returns, it means any of three things: the patient is biting into the tooth, there is still a significant amount of sensitive nerve material left in the tooth, or there is still more pus building up inside and around the infected tooth; all of these cause pain
Systemic issues
An infected tooth may endanger other parts of the body. People with special vulnerabilities, such as prosthetic joint replacement or mitral valve prolapse, may need to take antibiotics to protect from infection spreading during dental procedures. Both endodontic therapy and tooth extraction can lead to subsequent jaw bone infection. The American Dental Association (ADA) asserts that any risks can be adequately controlled. There is no scientific evidence that root canal therapy has any adverse affects on the overall health of the individual. Effective root canal therapy performed by adequately trained clinicians results in very high success rates with no systemic relationship to the patient's overall health.
If there is inflammation and swelling, the DENTAL SURGEON/ ENDODONTIST may prescribe an antibiotic or/and anti-inflammatory medicine for some days before starting the root canal procedure. The purpose is to control the infection and to ease the swelling which can make the anesthetic less effective.
If the condition is painful, the patient will have to take an over the counter or prescription analgesic to relieve the tooth pain until the procedure. The next step in the procedure is to take an X-ray to check the shape of the root canals and determine if there are any signs of infection in the surrounding bone
At the center of a tooth is a hollow area that houses soft tissue, known as pulp. This hollow area contains a relatively wide space towards the chewing surface of the tooth called the pulp chamber. This chamber is connected to the tip of the root of the tooth via thin hollow pipe-like canals—hence, the term "root canal". Human teeth normally have one to four canals, with teeth toward the back of the mouth having the most. These canals run through the center of the roots like pencil lead runs through the length of a pencil. The tooth receives nutrition through the blood vessels and nerves traversing these canals.
For patients, root canal therapy is one of the most feared procedures in all of dentistry; however, dental professionals assert that modern root canal treatment is relatively painless because the pain can be controlled. Lidocaine is a commonly used local anaesthetic. Pain control medication may be used either before or after treatment. However, in some cases it may be very difficult to achieve pain control before performing a root canal. For example, if a patient has an abscessed tooth, with a swollen area or "fluid-filled gum blister" next to the tooth, the pus in the abscess may contain acids that inactivate any anaesthetic injected around the tooth. In this case, it is best for the DOCTOR to drain the abscess by cutting it to let the pus drain out. Releasing the pus releases pressure built up around the tooth; this pressure causes much pain. The DENTAL SURGEON then prescribes a week of antibiotics such as penicillin, which will reduce the infection and pus, making it easier to anaesthetise the tooth when the patient returns one week later. The DENTAL SURGEON could also open up the tooth and let the pus drain through the tooth, and could leave the tooth open for a few days to help relieve pressure.
Steps of the Root Canal Procedure
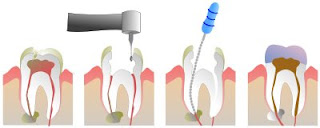
Root canal procedure'
1. Preparation for a root canal treatment
2. Anesthesia
3. Isolating the tooth
4. Gaining access to the dental pulp
5. Removal of PULP TISSUE
6. Measuring
7. Cleaning the root canals
8. Filling the root canals

Lower right first molar (center) after root canal therapy; the pulp chamber and root canals have been cleaned of debris, decontaminated and filled with gutta percha.
9.Restoring the Tooth After Root Canal
PULPECTOMY "pulpectomy" Sometimes the DENTAL SURGEON performs preliminary treatment of the tooth by removing all of the infected pulp of the tooth and applying a dressing and temporary filling to the tooth.
PULPOTOMY "pulpotomy" The DENTAL SURGEON may also remove just the coronal portion of the dental pulp, which contains 90% of the nerve tissue, and leave intact the pulp in the canals. This procedure, called a "pulpotomy", tends to essentially eliminate all the pain .
The pulpectomy and pulpotomy procedures eliminate almost all pain until the follow-up visit for finishing the root canal. But if the pain returns, it means any of three things: the patient is biting into the tooth, there is still a significant amount of sensitive nerve material left in the tooth, or there is still more pus building up inside and around the infected tooth; all of these cause pain
Systemic issues
An infected tooth may endanger other parts of the body. People with special vulnerabilities, such as prosthetic joint replacement or mitral valve prolapse, may need to take antibiotics to protect from infection spreading during dental procedures. Both endodontic therapy and tooth extraction can lead to subsequent jaw bone infection. The American Dental Association (ADA) asserts that any risks can be adequately controlled. There is no scientific evidence that root canal therapy has any adverse affects on the overall health of the individual. Effective root canal therapy performed by adequately trained clinicians results in very high success rates with no systemic relationship to the patient's overall health.
Saturday, September 20, 2008
THROAT INFECTIONS
The tonsils are areas of lymphoid tissue on either side of the throat. An infection of the tonsils is called tonsillitis. Most commonly, the term "tonsils" refers to the palatine tonsils that can be seen in the back of the throat.
Palatine tonsils are the tonsils that can be seen on the left and right sides at the back of the throat.
Tonsillitis is an inflammation of the tonsils and will often, but not necessarily, cause a sore throat and fever. In chronic cases tonsillectomy may be indicated.
Types
There are 3 main types of tonsillitis: acute, subacute and chronic.
Acute tonsillitis can either be bacterial or viral (75%)[citation needed] in origin.
Subacute tonsillitis (which can last between 3 weeks and 3 months) is caused by the bacterium Actinomyces.
Chronic tonsillitis, which can last for long periods if not treated, is almost always bacterial.
Acute tonsillitisTonsillitis is the inflammation of tonsils. Acute tonsillitis is the most common manifestation of tonsillar disease. It is associated with sore throat, fever, and dysphagia. The tonsils may appear normal sized or enlarged but are usually erythematous. Often, but not always, exudates can be seen. Not all these signs and symptoms are present in every patient.
Recurrent tonsillitis
Recurrent infection has been variably defined as from four to seven episodes of acute tonsillitis in one year, five episodes for two consecutive years or three episodes per year for 3 consecutive years.
Tonsillar hypertrophy
Tonsillar hypertrophy is the enlargement of the tonsils, but without the history of inflammation.

Obstructive tonsillar hypertrophy is currently the most common reason for tonsillectomy. These patients present with varying degrees of obstructive sleep and awake disturbances, which may include symptoms of loud snoring (accompanied by periods of irregular breathing), nocturnal choking and coughing, frequent awakenings with restless sleep, dysphagia, daytime hypersomnolence, and behavioral changes.Symptoms
Symptoms of tonsillitis include a severe sore throat (which may be experienced as referred pain to the ears), painful/difficult swallowing, headache, fever and chills, and change in voice causing a "hot potato" voice. Tonsillitis is characterized by signs of red, swollen tonsils which may have a purulent exudative coating of white patches (i.e. pus). There may be enlarged and tender neck cervical lymph nodes.
Causes
Bacterial tonsillitis may be caused by Group A streptococcal bacteria resulting in strep throat.
Viral tonsillitis may be caused by numerous viruses such as the Epstein-Barr virus (the cause of infectious mononucleosis) or the Adenovirus.
Sometimes, tonsillitis is caused by a superinfection of spirochaeta and treponema, in this case called Vincent's angina or Plaut-Vincent angina
Although tonsillitis is associated with infection, it is currently unknown if the swelling and other symptoms are caused by the infectious agents themselves, or by the host immune response to these agents. Tonsillitis may be a result of aberrant immune responses to the normal bacterial flora of the nasopharynx.
Treatment
Treatments of tonsillitis consist of pain management medications and lozenges.If the tonsillitis is caused by bacteria, then antibiotics are prescribed, with penicillin being most commonly used. Erythromycin is used for patients allergic to penicillin.
In many cases of tonsillitis, the pain caused by the inflamed tonsils warrants the prescription of topical anesthetics for temporary relief. Viscous lidocaine solutions are often prescribed for this purpose.
Ibuprofen or other analgesics can help to decrease the edema and inflammation, which will ease the pain and allow the patient to swallow liquids sooner.
When tonsillitis is caused by a virus, the length of illness depends on which virus is involved. Usually, a complete recovery is made within one week; however, some rare infections may last for up to two weeks.
Chronic cases may indicate tonsillectomy (surgical removal of tonsils) as a choice for treatment
 Throat with Tonsillitis
Throat with Tonsillitis

Throat after tonsillectomy

Two removed tonsils.
Complications

An abscess may develop lateral to the tonsil during an infection, typically several days after the onset of tonsillitis. This is termed a peritonsillar abscess (or quinsy).
Rarely, the infection may spread beyond the tonsil resulting in inflammation and infection of the internal jugular vein giving rise to a spreading septicaemia infection (Lemierre's syndrome).
In chronic/recurrent cases (generally defined as seven episodes of tonsillitis in the preceding year, five episodes in each of the preceding two years or three episodes in each of the preceding three years or in acute cases where the palatine tonsils become so swollen that swallowing is impaired, a tonsillectomy can be performed to remove the tonsils. Patients whose tonsils have been removed are certainly still protected from infection by the rest of their immune system.
Bacteria feeding on mucus which accumulates in pits (referred to as "crypts") in the tonsils may produce whitish-yellow deposits known as tonsilloliths. These may emit an odour due to the presence of volatile sulfur compounds.
Hypertrophy of the tonsils can result in snoring, mouth breathing, disturbed sleep, and obstructive sleep apnea, during which the patient stops breathing and experiences a drop in the oxygen content in the bloodstream. A tonsillectomy can be curative.
In very rare cases, diseases like rheumatic fever or glomerulonephritis can occur. These complications are extremely rare in developed nations but remain a significant problem in poorer nations.
Palatine tonsils are the tonsils that can be seen on the left and right sides at the back of the throat.
Tonsillitis is an inflammation of the tonsils and will often, but not necessarily, cause a sore throat and fever. In chronic cases tonsillectomy may be indicated.
Types
There are 3 main types of tonsillitis: acute, subacute and chronic.
Acute tonsillitis can either be bacterial or viral (75%)[citation needed] in origin.
Subacute tonsillitis (which can last between 3 weeks and 3 months) is caused by the bacterium Actinomyces.
Chronic tonsillitis, which can last for long periods if not treated, is almost always bacterial.
Acute tonsillitisTonsillitis is the inflammation of tonsils. Acute tonsillitis is the most common manifestation of tonsillar disease. It is associated with sore throat, fever, and dysphagia. The tonsils may appear normal sized or enlarged but are usually erythematous. Often, but not always, exudates can be seen. Not all these signs and symptoms are present in every patient.
Recurrent tonsillitis
Recurrent infection has been variably defined as from four to seven episodes of acute tonsillitis in one year, five episodes for two consecutive years or three episodes per year for 3 consecutive years.
Tonsillar hypertrophy
Tonsillar hypertrophy is the enlargement of the tonsils, but without the history of inflammation.

Obstructive tonsillar hypertrophy is currently the most common reason for tonsillectomy. These patients present with varying degrees of obstructive sleep and awake disturbances, which may include symptoms of loud snoring (accompanied by periods of irregular breathing), nocturnal choking and coughing, frequent awakenings with restless sleep, dysphagia, daytime hypersomnolence, and behavioral changes.Symptoms
Symptoms of tonsillitis include a severe sore throat (which may be experienced as referred pain to the ears), painful/difficult swallowing, headache, fever and chills, and change in voice causing a "hot potato" voice. Tonsillitis is characterized by signs of red, swollen tonsils which may have a purulent exudative coating of white patches (i.e. pus). There may be enlarged and tender neck cervical lymph nodes.
Causes
Bacterial tonsillitis may be caused by Group A streptococcal bacteria resulting in strep throat.
Viral tonsillitis may be caused by numerous viruses such as the Epstein-Barr virus (the cause of infectious mononucleosis) or the Adenovirus.
Sometimes, tonsillitis is caused by a superinfection of spirochaeta and treponema, in this case called Vincent's angina or Plaut-Vincent angina
Although tonsillitis is associated with infection, it is currently unknown if the swelling and other symptoms are caused by the infectious agents themselves, or by the host immune response to these agents. Tonsillitis may be a result of aberrant immune responses to the normal bacterial flora of the nasopharynx.
Treatment
Treatments of tonsillitis consist of pain management medications and lozenges.If the tonsillitis is caused by bacteria, then antibiotics are prescribed, with penicillin being most commonly used. Erythromycin is used for patients allergic to penicillin.
In many cases of tonsillitis, the pain caused by the inflamed tonsils warrants the prescription of topical anesthetics for temporary relief. Viscous lidocaine solutions are often prescribed for this purpose.
Ibuprofen or other analgesics can help to decrease the edema and inflammation, which will ease the pain and allow the patient to swallow liquids sooner.
When tonsillitis is caused by a virus, the length of illness depends on which virus is involved. Usually, a complete recovery is made within one week; however, some rare infections may last for up to two weeks.
Chronic cases may indicate tonsillectomy (surgical removal of tonsils) as a choice for treatment
 Throat with Tonsillitis
Throat with Tonsillitis
Throat after tonsillectomy

Two removed tonsils.
Complications

An abscess may develop lateral to the tonsil during an infection, typically several days after the onset of tonsillitis. This is termed a peritonsillar abscess (or quinsy).
Rarely, the infection may spread beyond the tonsil resulting in inflammation and infection of the internal jugular vein giving rise to a spreading septicaemia infection (Lemierre's syndrome).
In chronic/recurrent cases (generally defined as seven episodes of tonsillitis in the preceding year, five episodes in each of the preceding two years or three episodes in each of the preceding three years or in acute cases where the palatine tonsils become so swollen that swallowing is impaired, a tonsillectomy can be performed to remove the tonsils. Patients whose tonsils have been removed are certainly still protected from infection by the rest of their immune system.
Bacteria feeding on mucus which accumulates in pits (referred to as "crypts") in the tonsils may produce whitish-yellow deposits known as tonsilloliths. These may emit an odour due to the presence of volatile sulfur compounds.
Hypertrophy of the tonsils can result in snoring, mouth breathing, disturbed sleep, and obstructive sleep apnea, during which the patient stops breathing and experiences a drop in the oxygen content in the bloodstream. A tonsillectomy can be curative.
In very rare cases, diseases like rheumatic fever or glomerulonephritis can occur. These complications are extremely rare in developed nations but remain a significant problem in poorer nations.
Subscribe to:
Comments (Atom)


